ARVO 2024 presentation: Synthetic Peptide Hydrogel-Based Human In Vitro Corneal Model
INTRODUCTION: Synthetic peptide hydrogels are promising scaffolds where cornea epithelium and other cell types can be grown into in vitro cultures. The aim of this study was to develop a corneal model employing a peptide hydrogel layer as a mimetic of corneal stroma. The model was used in the assessment of corneal cytotoxicity and penetration properties of prostaglandin analogs that are considered as first-line treatment for glaucoma.
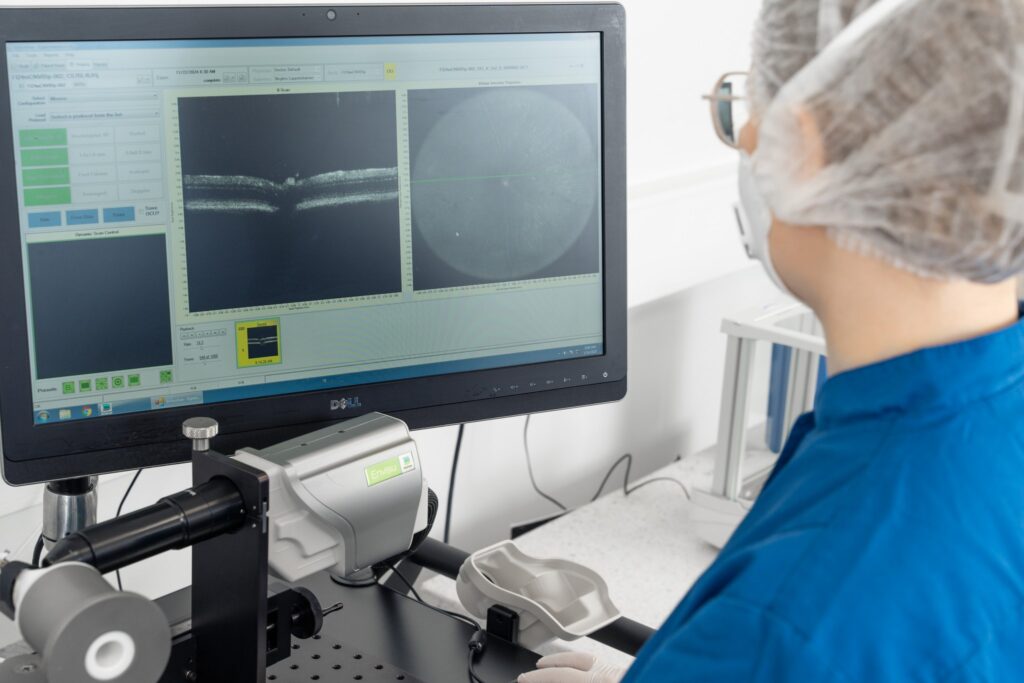
MATERIALS AND METHODS: The hydrogel was produced from human collagen-mimetic peptides1 exhibiting relevant properties. The hydrogels were cast into microplate wells and cell culture inserts. Human corneal epithelial cells (HCE-T) (Riken, Tsukuba, Japan) were seeded on the hydrogels and multilayered for the permeability experiments using the air-liquid interface method. In the cell viability experiments, the plastic-based conventional microplate cultures were used as a control condition. Cytotoxicity of benzalkonium chloride (BAK), vehicle (0.5% DMSO) and prostaglandin analogues, bimatoprost, latanoprost, tafluprost and travoprost (50 µM in 0.5% DMSO), were assessed using PrestoBlue (Thermo Fisher Scientific, Waltham, MA, USA) and lactate dehydrogenase (LDH) release assays. The permeability of fluorescent reference molecules, i.e., FITC-dextran 70 kDa and 4 kDa, Rhodamine 123, 6-carboxyfluorescein and Rhodamine B, and prostaglandin analogues was measured according to previously reported methodology2. Statistical significance of differences was tested by one-way ANOVA followed by Dunnett’s multiple comparisons test using Prism 10 (GraphPad Software, Boston, MA, USA).
RESULTS: There was a clear dose-response in the cytotoxicity at clinically relevant BAK concentrations. The IC50 values of BAK in HCE-T cells grown in plastic microplates were slightly lower (0.0056%) than on hydrogels (0.0079%). Latanoprost, tafluprost, travoprost and positive control BAK (0.01%) significantly decreased the cell viability on microplates (P<0.0001) and on hydrogels (P<0.05 latanoprost, P<0.01 tafluprost, P<0.01 travoprost, P<0.0001 BAK). Nevertheless, the cell viability was maintained relatively high (>72% on microplates, >86% on hydrogels) with all tested prostaglandin analogues. The apparent permeability coefficient (Papp) values between prostaglandin analogues were different. Tafluprost and travoprost showed very low Papp values. On the contrary, latanoprost and bimatoprost were identified as high permeability molecules with high Papp values.

Figure 1. Cell viability, LDH release, permeability values and mass balance of studied active compounds: Tafluprost, Travoprost, Latanoprost and Bimatoprost.
CONCLUSIONS:
1. HCE-T cells grown on human collagen-mimetic peptide hydrogels that mimic the stroma are suitable as a corneal in vitro model.
2. The model is convenient for the assessment of cytotoxicity and permeability of ophthalmic drugs in early phase of drug discovery.
Authors: Dovilė Litvinavičiūtė | Justina Urbanavičiūtė | Tadas Jelinskas | Airinė Mazėtytė-Godienė | Vytautas Cėpla | Rūta Aldonytė | Jenni J. Hakkarainen
Keywords: Cornea, Hydrogel, Cell viability, Permeability
Check out our latest news and activities
All Scientific publications


Copyright: Experimentica Ltd. 2025