ARVO 2024 presentation: Validating injectable anesthesia for the streptozotocin-induced diabetic retinopathy rat model
INTRODUCTION: Streptozotocin (STZ) induced hyperglycemic rats, commonly used in preclinical diabetic retinopathy (DR) research, have poor response to the most used laboratory rodent anesthesia, medetomidine / ketamine mixture (MK), necessitating higher doses, prolonged recovery periods, and heightened mortality risk (1,2,3). The objective of this study was to assess a fully reversible injectable anesthesia protocol, medetomidine-midazolam-butorphanol (MMB), in the STZ-induced DR rat model with the aim to reduce the MK adverse effects without compromising the DR model development.
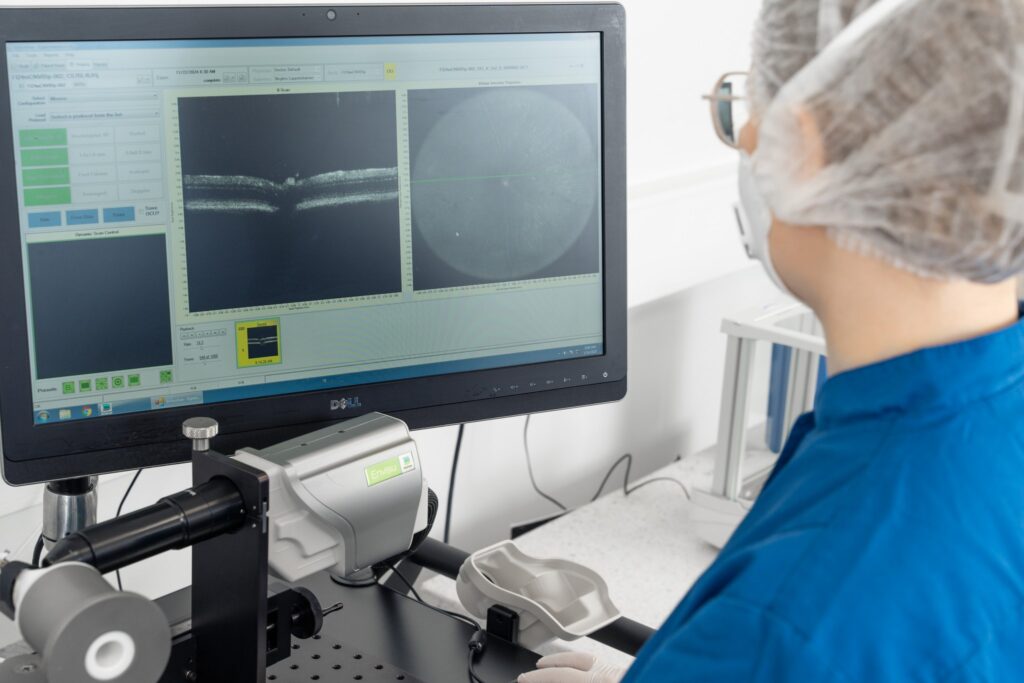
MATERIALS AND METHODS: Two groups (n=14/group) of male 8-week-old outbred RjHan:SD rats (Janvier Labs), were induced with two IP injections of STZ (32.5 mg/kg, Day 0 & Day 2) in sodium citrate buffer. Two groups of rats (n=11/group) were administered buffer alone (Sham). The DR pathology was evaluated with cataract scoring and scotopic flash electroretinography (ERG) at Weeks 4, 6, 8, and 14. The rats were anesthetized for the ERG with either MMB (0.15, 2.0, 2.5 mg/kg) or MK (0.3, 40.0 mg/kg). MMB was reversed with a mixture of atipamezole, flumazenil, and naloxone (0.75, 0.2, 0.12 mg/kg), and MK was reversed with atipamezole (1.0 mg/kg).
RESULTS: Clinical health scoring indicated better body weight maintenance and lower distress levels in MMB groups compared to the MK groups. At Week 14 the blood glucose levels were 5.8±0.5 (sham+MMB), 5.7±0.7 (sham+MK), 27.7±6.7 (STZ+MMB), and 29.6±7.0 (STZ+MK) mmol/l. The STZ induced rats anaesthetized at Week 14 with MMB showed a significant reduction in the flash ERG b-wave amplitude at 1, 3, and 10 cd.s/m2 luminance (Fig. 1). A similar trend was seen with the main OPs.

Figure 1. At Week 14, there was a delay in the a-wave latency of STZ induced rats compared to the Sham groups with corresponding anesthesia. Oscillatory Potentials (OPs) showed significant delay already at Week 4. Mixed-effects analysis with Holm-Šídák’s multiple comparisons test. */#, P<0.05; **/##, P<0.01; ***/###, P<0.001. Similar results were seen with 1 and 10 cd.s/m2.
The incidence of cataracts was slightly higher in STZ-induced DR rats with MK anesthesia than in STZ-induced DR rats with MMB anesthesia at weeks 12 and 14 post-induction of DR (Fig. 2).

Figure 2. The incidence of cataracts during the follow-up period of STZ-induced DR rats.
CONCLUSIONS:
1. The RjHan:SD strain chosen for the experiments is extra sensitive to the MK anesthesia, confirming previously published data (3).
2. The development of the DR phenotype was not affected with the use of MMB.
3. MMB proved to be suitable injectable anesthesia for hyperglycemic rats, having faster recovery, reduced mortality, and less adverse effects than the standard MK anesthesia.
Authors: Anni Tenhunen | Leena Tähtivaara | Heidi Koskenniemi | Birgitta Lappeteläinen | Päivi Partanen | Anna Mari Koponen | Xavier Ekolle | Anni Kolehmainen | Satu Mering | Hanna-Marja Voipio | Marc Cerrada-Gimenez
Keywords: Streptozotocin, Diabetic Retinopathy, Animal Welfare
Check out our latest news and activities
All Scientific publications


Copyright: Experimentica Ltd. 2025